Synergy Expert Meeting
The annual Synergy Expert Meeting is organised to provide an opportunity for synergistic discussion between health psychologists conducting research in core fields within health psychology. The focus is on advancing the standard of work within the field by pooling expertise, sharing critical evaluations, and stimulating networking and collaborative research between researchers from all over Europe in an informal and supportive atmosphere. The aim is to develop improved theoretical and methodological approaches, as well as practical applications in respect of the Synergy Expert Meeting topic. It is an opportunity for researchers to present their research for discussion in depth with other experts working in the same field in a friendly and relaxed atmosphere. By focusing on a core topic on which all participants have some expertise and have conducted research (published and unpublished), we would expect to reach a shared understanding of the strengths, weaknesses and opportunities in the area. We hope that this will influence future research and its application in the field.
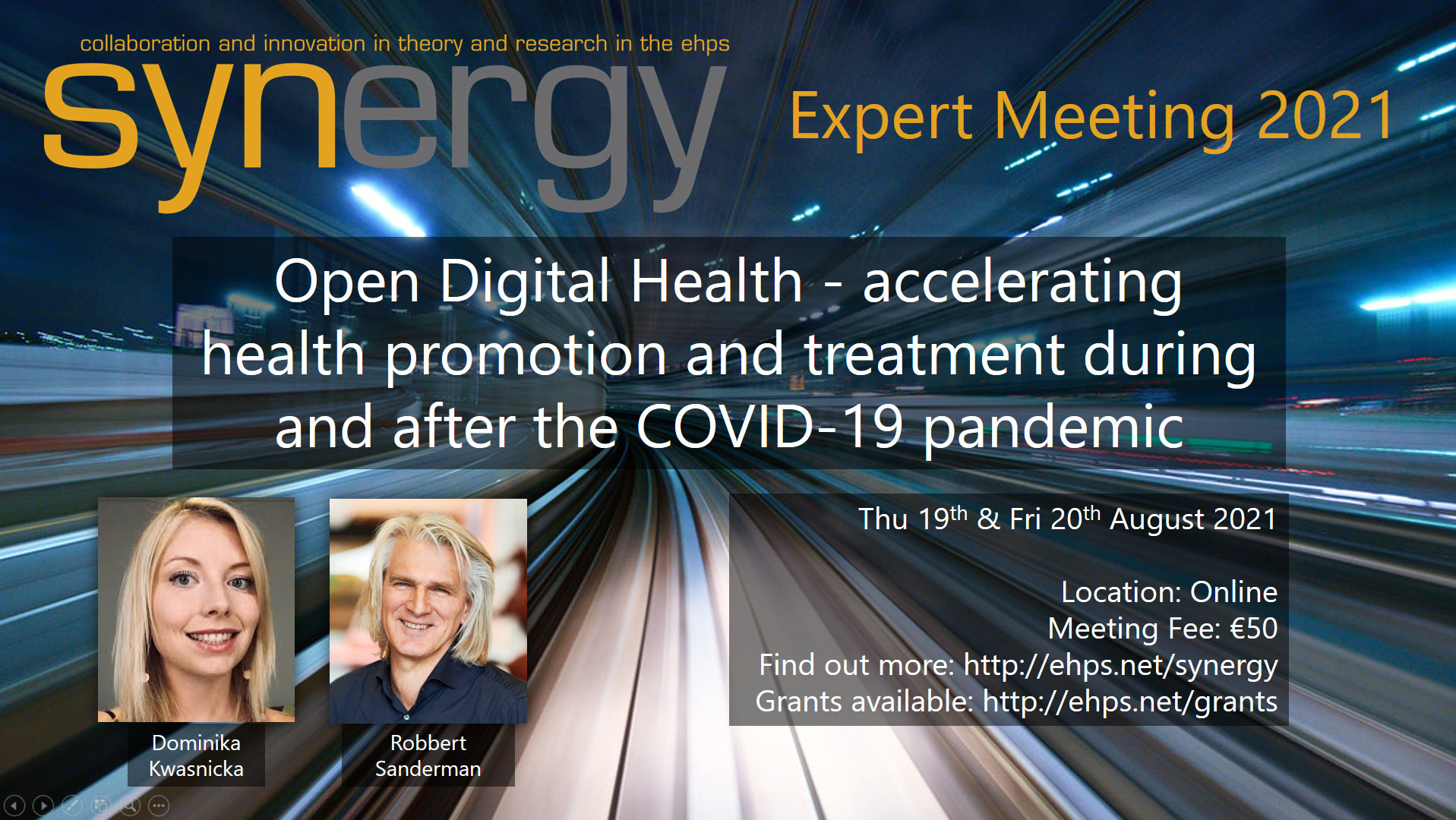
Open Digital Health – accelerating health promotion and treatment during and after the COVID-19 pandemic
Conference format: Online
Facilitators: Dominika Kwasnicka and Robbert Sanderman
Regular fee: €50
Fee waiver: Please contact us (ehps.synergy@gmail.com) for a reduced fee (€30) if you are a member of a member of a lower-middle-income country (For a list of eligible countries click on the following link: worldbank rating)
Please apply here: Google Forms Link
Application deadline: 23/07/21
Event dates: Thursday 19th August and Friday 20th August, 9am CET start time. First session 9-11am. One-hour break. Second session 12-2pm CET. On Friday at 2pm social event.
Title: Open Digital Health – accelerating health promotion and treatment during and after the COVID-19 pandemic.
The aim of this Synergy Expert Meeting is to stimulate discussion around the implications and applications of Open Digital Health tools for health psychology research and practice. The objectives are to identify the most pertinent methods and strategies for applying and evaluating open digital health tools, especially the ones that are used in research, prevention and treatment in relation to health psychology domains.
We aim to jointly write a manuscript setting out the research agenda arrived at within the meeting, and to formulate plans for methodologically rigorous research to pursue this agenda. At the meeting we will debate methods for Open Digital Health tools validation and we will outline the best strategies to reuse them across different populations and settings. The participants of the meeting will discuss three key elements of open digital health tools’ sharing: (1) data; (2) content; (3) codes and design features. We will discuss and elaborate on the pros and cons of openly sharing each of them.
In the recommendations statement that we would ask the participants to co-author, we will outline from the perspective of health psychology:
- What are the methods in our health psychology research toolkit that can be best used for testing and evaluating digital health tools?
- What are the most feasible strategies to reuse digital health tools across contexts, populations and settings?
- What are the main advantages and disadvantages of sharing (openly publishing) data, content and codes and design features of digital health tools?
We will give actionable suggestions for the researchers on the topic of what they can do in order to join the continuously growing Open Digital Health movement and we will also explore what pitfalls they need to be aware of and avoid. We will also position our discussion in the current context of COVID-19 pandemic, exploring how digital health tools rapidly gained popularity in 2020-2021 when world-wide health promotion and health treatment efforts shifted from face-to-face to online delivery. We will explore what are the opportunities and challenges of the Open Digital Health revolution that we are expecting in the coming years.
Set-up of a collaborative expert meeting: The meeting thread will largely depend on participants’ research interests and priorities, and we will ask attendees to share their key interests and topics they are the most interested in prior to the meeting. We will set up a meeting that is highly interactive and feasible to deliver online. In the past, Synergy Expert Meetings were two-day events that aimed to enhance networking, progressing of ideas and in-person interactions. This year will be no different, although we will use the internet as a communication medium. The participants of the meeting will be asked to fully commit to the meeting, they will receive an information and care pack before the meeting with relevant materials and items needed for the meeting.
Activities: Staying online for prolonged times is not ideal for mental and physical health, therefore, the meeting will be divided into short bursts, including information exchange, discussions, small group debates, brainstorm boards, and voting. In total we will have 4 x 2-hour sessions. We will have an active break in the middle of each day giving participants an hour to have lunch, go for a walk, stretch, do yoga etc. On the final day we will also encourage meeting participants to stay online after the meeting ends, for a social part of the meeting. This one is kept as a surprise and will be prepared by the Synergy Organising Board.
Expert meeting outcomes: The key outcome of the Synergy Expert Meeting is networking and creating opportunities for future collaborations and projects. The secondary outcome is a consensus statement. We are keen to achieve the consensus on some of the issues discussed and as customary for the Synergy Expert Meeting we would like to collaboratively write a consensus statement (to be submitted to a peer-reviewed journal) that will summarise the meeting outcomes together with all meeting participants and with the Open Digital Health leadership team. We expect that people who are experts in digital health will attend the meeting. Please tell us about your expertise on the topic when you fill in your application form.
Facilitators
Dominika Kwasnicka (University of Melbourne and SWPS University) and Robbert Sanderman (University of Groningen and University of Twente) are both Directors of Open Digital Health Foundation. This year they jointly co-edited a book “Psychological Insights for Understanding COVID-19 and Health” (Routledge, 2021). They have both been strongly involved in the EHPS, Dominika is a past Chair of Synergy and a current Executive Board Member of the EHPS EC and Robbert is a Fellow and Past President of the Society. They are both passionate about making digital health more accessible, more scalable and more equal for all. This year Synergy Expert Meeting will also have five co-facilitators, other acting Directors of the Open Digital Health Foundation who will join the group of experts and will lead small group discussions and debates: Gill ten Hoor (University of Maastricht), Olga Perski (University College London), Jan Keller (Freie Universität Berlin), Gjalt Jorn Peters (Open University, the Netherlands), and Sebastian Potthoff (Northumbria University). They are all digital health experts and long-term active members and supporters of the EHPS.
Description: Digital health tools, defined broadly as any technology-supported tools used to promote health and wellbeing, can improve disease prevention and healthcare delivery at the population-level. These may include remote consultations, smartphone apps, websites, wearables, and external monitors. Digital health tools are rapidly becoming a norm in healthcare provision but their proliferation poses multiple challenges. The omnipresence of mobile and wearable devices gives them the potential to effectively deliver health promotion interventions and support behaviour change. This potential is widely recognised by public health bodies across the globe, with national and international policy efforts to stimulate digital health innovation and regulation. The COVID-19 pandemic has further emphasised the urgency of a digital health revolution, with digital health tools touted as a vital means to alleviate pressure on health and social care systems.
The potential of digital health tools notwithstanding, key issues lie in their evaluation and scalability: although some tools are clearly effective, their robust evaluation and successful implementation remain limited to specific geographical settings and specific diseases. Consequently, digital health tools have yet to significantly impact health and wellbeing at the population level (Gordon et al, NPJ Digital Medicine, 2020). To achieve their full potential, digital health tools need to be better evaluated, integrated and effectively scaled. This Synergy Expert meeting will aim to address two specific, closely connected issues that will be explored and discussed during the meeting:
(1) Fit-for-purpose validation is lacking. Although a plethora of digital health tools are available on the market, only a fraction of these has been rigorously evaluated in clinical trials (Zhao et al., JMIR, 2016). Data from IQVIA confirms this – as of 2017, only 0.18% of 325,000 published health apps on consumer platforms had undergone formative evaluation. Although early iterations of evidence standards frameworks for digital health are available from institutions such as the European Commission, the UK Medicines and Healthcare products Regulatory Agency, and the US Food and Drug Administration, the number of digital health tools that have undergone rigorous evaluation is low. The underlying problem is that the randomised controlled trial (RCT) is seen as the gold-standard evaluation method. Although RCTs are powerful, they are not always fit-for-purpose in the context of digital health tools. The lengthy, costly and strict setup of RCTs somewhat contradicts the intrinsic qualities of digital health tools, including their speed of development, affordability, agility and relatively fast real-world use. There is hence an urgent need to supplement and expand the toolbox of methods available for evaluating the effectiveness of digital health tools.
(2) Digital health tools are not reused in different contexts and populations. This drastically limits the health and societal impact of the international digital health community. In practice, the duplication of efforts and development of new tools from scratch means time and resources are often wasted (e.g., converting sensor input to relevant self-monitoring data, creating feedback algorithms, developing persuasive design elements or tailored content). This duplication of effort is particularly wasteful in the context of digital health tools: a key advantage of digital health tools is their potential for reuse, either as a whole or in part, as they are typically modular in structure with source code, content, and algorithms easy to share, modify or build onto.
The interconnection between the lack of fit-for-purpose validation methods (the first issue) and appropriate reuse (the second issue) becomes apparent when considering the following: digital health tools are typically validated in specific contexts, i.e., in a specific country/region within a specific healthcare system and/or with a small subgroup of patients (partially because of the costs of RCTs). In addition, none of the extant curated health app portals and repositories (e.g., the UK National Health Service’s Apps Library) include direct links to the underlying evidence and/or well-defined descriptions of the contexts in which they were developed and evaluated (e.g., using the TIDieR checklist, Hoffmann et al., BMJ, 2014). For developers, researchers, clinicians, payers, and users, it is hence currently impossible to assess which of the myriad available digital health tools is appropriate for their specific purpose. Consequently, many developers and researchers choose to build a new tool from scratch, thus resulting in a highly fragmented digital health ecosystem with poorly validated and often not scalable digital health tools. The aim of the Open Digital Health initiative is to give these digital health tools ‘a second life’ by promoting the reuse of existing evidence-based tools and their application across different contexts and settings. We expect this will ultimately help decrease costs and increase the reach of existing digital health tools. By doing so, the Open Digital Health team aims to systematise, better integrate and scale existing digital health tools nationally and internationally.
Selected references:
- Sullivan, I., DeHaven, A., & Mellor, D. (2019). Open and reproducible research on open science framework. Current Protocols Essential Laboratory Techniques, 18(1), e32.
- Nosek, B. A. (2014). Improving my lab, my science with the open science framework. APS Observer, 27(3).
- Laffey, J. G., & Kavanagh, B. P. (2018). Negative trials in critical care: why most research is probably wrong. The Lancet Respiratory Medicine, 6(9), 659-660.
- Nosek, Brian A., George Alter, George C. Banks, Denny Borsboom, Sara D. Bowman, Steven J. Breckler, Stuart Buck et al. “Promoting an open research culture.” Science 348, no. 6242 (2015): 1422-1425.
For further information please contact: ehps.synergy@gmail.com